
People with conditions like cancer, heart disease, diabetes, HIV, and overweight and obesity face a much higher risk of death from COVID-19. That is why people with conditions like this, also called existing comorbidities, were initially prioritized for the first round of COVID-19 vaccination in March 2021. The goal was to reach 500,000 people with co-morbidities within the first five months. Yet, vaccine uptake is low for people with these conditions, only reaching 5% of the target. To understand why, IDI studied what keeps people from receiving the recommended vaccine (barriers) and what factors contribute to following through with vaccine recommendations (enablers).
To better understand barriers and enablers to COVID-19 vaccine use among people with existing comorbidities, IDI engaged stakeholders, represented by organizations including the Uganda Diabetic Association, Community Health and Information Network, Uganda Cancer Institute, Uganda Heart Institute, Uganda Association of Physicians, and the National Umbrella Organization for People Living with HIV in Uganda, among others among other groups to help. Through the engagements, IDI asked stakeholders to help us identify COVID-19 vaccination barriers and enablers. IDI also worked closely with these groups to develop messages for people with comorbidities. IDI also worked with these groups to develop a strategy to get COVID-19 vaccination messaging designed especially for the vulnerable group into the media, including television broadcasts.
Through these efforts, IDI and our partners conceived, developed, and implemented a new Vaccination at Point of Care Model. This Innovation extends outreach services to health facilities where people with comorbidities routinely access treatment—reaching people where they are with potentially lifesaving information and resources.
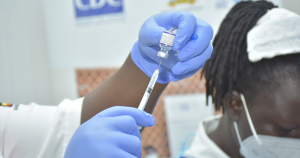 To see whether this new approach would work, IDI and our partners piloted this new vaccination model first at the Mulago HIV prevention, care, and treatment clinic(PCT). This urban care facility in Kampala provides care to more than 8,000 people living with HIV. The Mulago facility usually sees each patient once every three months for routine care. To begin, IDI trained clinic staff to become vaccination champions. These champions focused on strengthening advocacy within the clinic. Vaccination champions worked with other staff and caregivers to ensure they were equipped to counter misinformation about the COVID-19 vaccine. IDI set up a coordination team among the staff to be sure vaccination teams could be well integrated into the clinic schedule and to be sure that the right data could be properly collected.
To see whether this new approach would work, IDI and our partners piloted this new vaccination model first at the Mulago HIV prevention, care, and treatment clinic(PCT). This urban care facility in Kampala provides care to more than 8,000 people living with HIV. The Mulago facility usually sees each patient once every three months for routine care. To begin, IDI trained clinic staff to become vaccination champions. These champions focused on strengthening advocacy within the clinic. Vaccination champions worked with other staff and caregivers to ensure they were equipped to counter misinformation about the COVID-19 vaccine. IDI set up a coordination team among the staff to be sure vaccination teams could be well integrated into the clinic schedule and to be sure that the right data could be properly collected.
The pilot was a success. In just nine months, nine out of every 10 patients at the Mulago clinic have been screened for their current vaccination status and seven out of ten had received their first dose of COVID-19 vaccine; half of them through the new point of care pilot. The project also generated good information about why people declined the COVID-19 vaccine. Among the 1000+ that declined to be vaccinated, fears related to side effects, pregnancy and breastfeeding, and interfering with treatment or other health conditions topped the list. The information gained through this pilot will help other PEPFAR-supported projects implement what works to increase COVID-19 vaccination. The pilot has also generated information needed to inform new strategic thinking and decision-making in HIV programming in Uganda.
This pilot shows us two key lessons. First, extending vaccination at healthcare facilities where the most vulnerable patients are already accessing chronic care allows for better acceptance of vaccination services by this population category as this is being recommended by their routine care-gives. Second, the pilot also demonstrates that patients are more confident receiving vaccination services where they already get care. They trust that their caregivers will provide them with information relevant to their conditions in relation to vaccination.
Plans are underway to ensure 100% full and booster vaccination coverage within the clinic and scale-up of the implementation strategies used in PCT to all PEPFAR clinics countrywide.






